This week’s news story highlights the contribution of Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST) and Prof. Radhakrishnan’s work in particular who also happens to be the senior author of the epidemiological tudy presenting the rise of neurological disorders in India (see previous news story).
Turns out, the institute researches different facets of neurological disabilities in an Indian context to produce directly relevant, implementable and cost-effective solutions. Probably, the most notable is the establishment of R. Madhavan Nayar Center for Comprehensive Epilepsy Care at SCTIMST. It has become one of the leading centres for epilepsy care outside North America and Europe and has undertaken over 1200 surgical procedures for epilepsy over the past 17 years. Under Prof Radhakrishnan’s direction, SCTIMST has pioneered advanced neurological therapies in India, such as epilepsy surgery and deep brain stimulation. They have achieved excellent outcomes comparable with the best centres of the world and all this has been done at a fraction of the cost abroad (1,2).
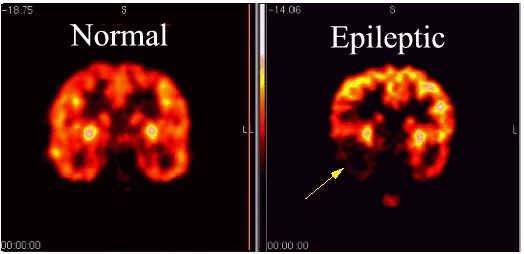
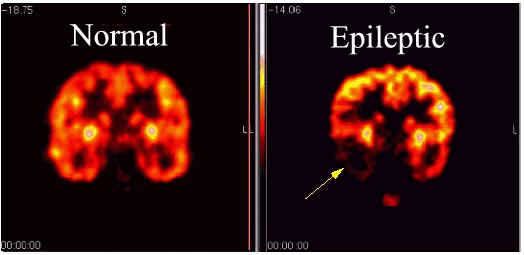
By reviewing data of all patients who had undergone presurgical evaluation at Madhavan Nayar Center for Comprehensive Epilepsy Care between 2005 – 2008, following up with these patients post-surgery and taking their economic background into consideration, they have proposed considerations for performing a cost-effective epileptic surgery. Selection of patients with identified lesions was found to lead to a favourable seizure-free postoperative outcome. In cases, where MRI scans cannot detect a lesion, invasive monitoring needs to be used. In India, health insurance doesn’t cover epilepsy care. Mean cost of surgery and hospitalisation amounts to INR 60,000 with invasive monitoring increasing the cost to INR 1,37,000 (3). This precludes invasive monitoring usage to affluent patients only. The same is reflected in the study where 40⁄214 patients could not proceed further with the surgery because of their inability to afford invasive monitoring. Of note, the cost at this centre is still a fraction compared to cost in USA or in Europe.
Under such conditions the authors conclude that in order to achieve excellent results under minimum cost, it is best to select patients whose lesions can be distinctly identified using MRI alone (4). In another study, SNP rs3812718 associated with higher incidences of epileptic seizures in Caucasian patients was probed for distribution and epilepsy association in South Indian patients. 203 epileptic patients of Kerala origin who had undergone surgery and were seizure-free for at least two years following surgery formed the study group. 282 people also of Kerala origin who didn’t have any neurological disorder were chosen as control. Genotyping of these two populations and statistical analysis showed that contrary to European population, SNP rs3812718 doesn’t contribute to development of epileptic seizures in Kerala population. This shows the need to identify population specific biomarkers to aid early diagnosis of neurological disorders (5).
On the treatment side, a survey of physiotherapists in the state of Kerala showed variation of treatment approaches in stroke rehabilitation programmes. Uses of walking aids and involvement of the physiotherapist in discharge of the patient were found to be contentious issues. This underlines the need to put a standardised rehabilitation programme in place (6).
The success of SCTIMST in a highly complex case like epilepsy surgery, exemplifies how excellence can be achieved through planning, research and manpower development in Indian healthcare. Availability of newer MRI techniques, companies designing cheaper diagnostic tools, collection of population specific genomic data is sure to make a dent on costs.
However, the first step would be recognition and sensitisation to the problem which can only be achieved by promoting awareness of neurological disorders by education.
Further reading:
- Radhakrishnan K. Challenges in the management of epilepsy in resource-poor countries. Nat Rev Neurol. 2009 Jun;5(6):323 – 30.
- Singh VP. Epilepsy surgery in India. J Pediatr Neurosci. 2011 October; 6(Suppl1): S130 – S134.
- Chaudhry N, Radhakrishnan A, Abraham M, Kesavadas C, Radhakrishnan VV, Sankara Sarma P, Radhakrishnan K. Selection of ideal candidates for extratemporal resective epilepsy surgery in a country with limited resources. Epileptic Disord. 2010 Mar;12(1):38 – 47.
- Dash GK, Radhakrishnan A, Kesavadas C, Abraham M, Sarma PS, Radhakrishnan K. An audit of the presurgical evaluation and patient selection for extratemporal resective epilepsy surgery in a resource-poor country. Seizure. 2012 Jun;21(5):361 – 6.
- Balan S, Vellichirammal NN, Banerjee M, Radhakrishnan K. Failure to find association between febrile seizures and SCN1A rs3812718 polymorphism in south Indian patients with mesial temporal lobe epilepsy and hippocampal sclerosis. Epilepsy Res. 2012 Sep;101(3):288 – 92. doi: 10.1016/j.eplepsyres.2012.04.009.
- Khan FR, Vijesh PV, Rahool S, Radha AA, Sukumaran S, Kurupath R. Physiotherapy practice in stroke rehabilitation: a cross-sectional survey of physiotherapists in the state of Kerala, India. Top Stroke Rehabil. 2012 Sep-Oct;19(5):405 – 10.
- Image Source: http://neurosciencefundamentals.unsw.wikispaces.né…